Not really worried about taking expired medicines? Here are 6 things you should know
A fair few Singaporeans have taken expired medication. Does it seem to work most of the time, or do we just tell ourselves that? The programme Talking Point looks into the efficacy and safety of drugs past their expiry date.

Do you store medication at home? Ever notice the expiry dates?
SINGAPORE: Sometimes when her body aches, Humaira Sulaiman takes the painkillers she keeps in her fridge.
Some of her medications, including for flu and coughs, are past their expiry date by as much as two years. But that is not something she checks.
“Maybe I tell myself (they work),” she said. “Most of the time … (they seem) to work.”
Another Singaporean, Oskar Song, knows he has taken expired medication. Some of his medicine boxes are yellowing, and the expiry dates have faded. But he is “not really” worried about the side effects. “I’m still alive,” he quipped.
The two of them are not the only ones with no qualms about storing medicines past the expiry dates.
In a Talking Point poll on Instagram, 33 per cent of the 708 respondents said they have taken expired medication. Another 19 per cent said they did not check expiry dates when taking their medicines.
But do expired medications still work as intended? Are they even safe to consume? Here are six things you should know the next time you have a runny nose, headache or allergy symptoms.
WATCH: Is expired medicine still safe to consume? (22:02)
1. WHAT IS THE SHELF LIFE OF MEDICINES?
Different medicines have different shelf lives. For tablets and capsules, “it can be as short as six months” and “as long as five years”, according to Priscilla Lim, the managing pharmacist of The Pharmacy Inc.
For liquids, it is two years on average, and one to two years for eye drops.
Compounded medications, which are custom-made for a patient’s “unique needs”, typically have a shorter shelf life — up to six months — “because they’re made from scratch”, said Lim.
Some medications have a longer shelf life “because they’re chemically more stable”. They can withstand change arising from contact with other chemicals or the environment — more so than medicines that are chemically not stable, which “may degrade faster”, she said.

The shelf life of an unopened product is also different from that of an opened product. A bottle of eye drops, for example, is sterile when unopened, which means there are “no germs at all in the product”.
“Once you open it, it’s no longer sterile,” Lim said. And the product usually must be discarded within 30 days, she advised.
2. HOW EFFECTIVE ARE EXPIRED MEDICINES?
To find out the efficacy of expired medicines, Talking Point sent samples to a laboratory for tests: Two types of painkillers, two types of antihistamines — which are used to treat allergies — and a cough mixture.
Of the five, which all had expired for at least a year, four passed the test. Those drugs retained a 90 per cent potency level. The sample that failed, a painkiller in syrup form, had a 51 per cent potency.
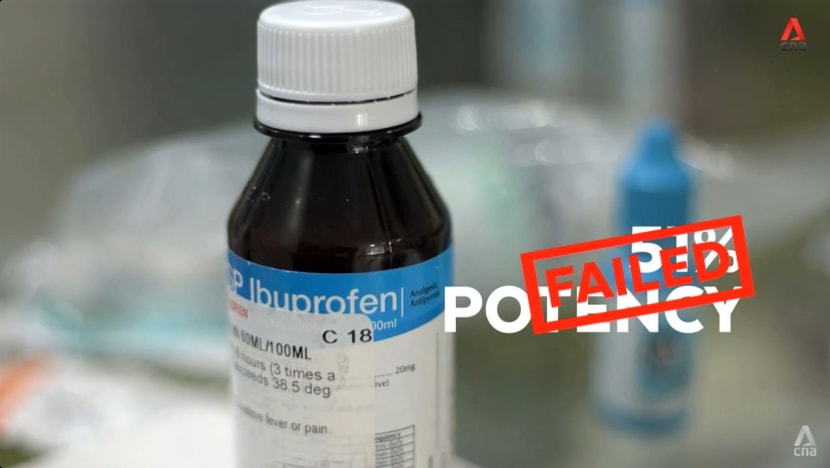
For medicines to be considered effective, manufacturers set the level of potency at above 90 per cent.
A drug’s efficacy past its expiry date may be affected, however, by storage conditions, which are an “important variable”, said Lita Chew, who heads the National Cancer Centre Singapore’s pharmacy department.
Tests done by the United States Food and Drug Administration to extend the shelf life of drug products stockpiled by the US military have shown that the stability of some drugs can be extended beyond the labelled expiry dates.
About 88 per cent of the expired drugs, representing 122 drug products, were deemed potent enough to be kept for at least a year beyond their original expiry date.
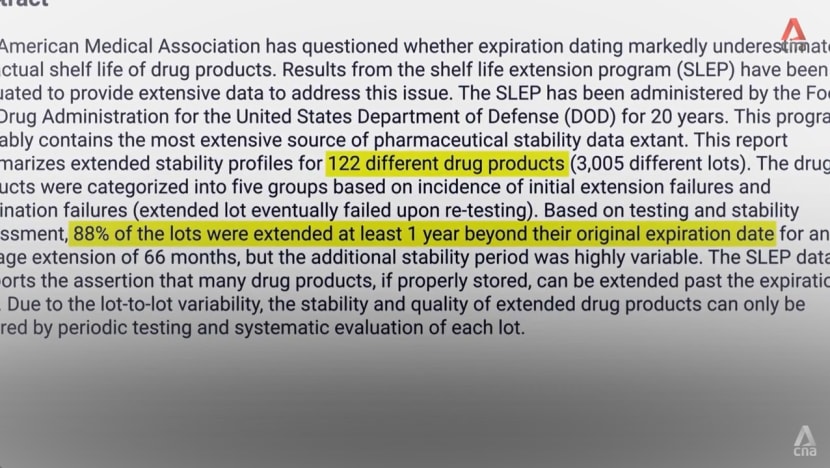
The drugs had been kept, however, in their original sealed packaging before testing — and in a “very controlled environment”, pointed out Chew, who cautioned against extrapolating results from this US programme to consumers.
“We don’t keep our drugs in that kind of condition,” she said. “That’s why regulators out there still recommend that … (consumers) discard expired medication.
Medication will start to degrade the moment it leaves the manufacturing plant. (The question is) how fast it degrades. So I’d still advise people to stick to the … expiry date to assure optimal efficacy.”
3. WILL REFRIGERATION MAKE A DIFFERENCE?
Some people store their medicines in the fridge. But the best thing to do is check the label for storage instructions. Some medications may damage because of the cold and are best stored between 15 and 25 degrees Celsius instead.
This means avoiding places that collect heat, such as beside the oven or the fridge, and looking for a cool, dry place, like a drawer or a shelf.
In Singapore’s hot weather, however, that is not always possible, noted Singapore General Hospital principal pharmacist Ong Kheng Yong.
“We’ve done a small experiment, and the temperatures at home can range (up to) as high as 30 to 31 deg C,” he said. “Under these less-than-ideal conditions, there’s a chance that the medication may deteriorate faster than it should.
“That brings down its shelf life, and it may not last all the way till its expiry date.”

4. WHAT ARE THE RISKS WHEN MEDICINES DEGRADE?
Common medicines that people store at home include cough syrup, nasal spray, antifungal and steroid creams as well as eye drops.
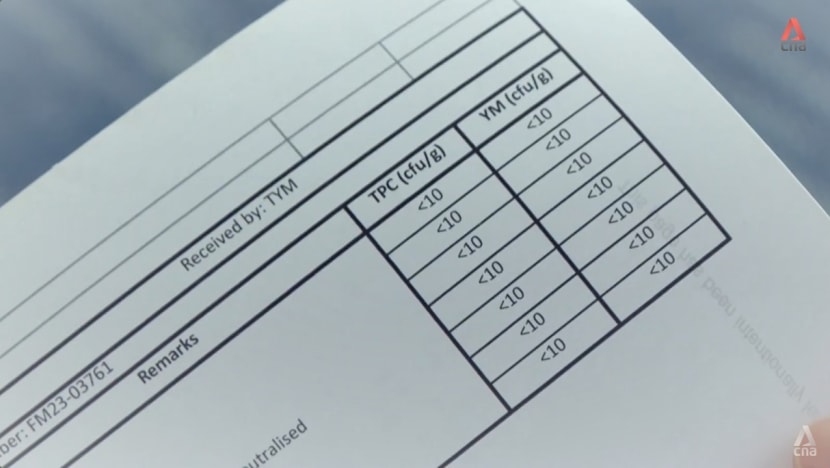
These medicines are also at risk of bacterial contamination, so Talking Point sent seven samples to another laboratory to be tested for safety.
The samples had been opened for more than 30 days, most of them were at least a year past their expiry date, but the tests showed that their total plate count, which encompasses most bacteria, was less than 10 each.
This meant there was no bacterial growth, even in two samples that had expired in 2018 and in 2019. The reason is “all these products would have preservatives”, said Chew.
“Preservatives create a very hostile environment for micro-organisms, like bacteria … and moulds, to grow (in).”
But she does not recommend, for example, using eye drops past the expiry date. If the bottle is frequently opened and closed, “the chances of contamination are very high”.
“When you have too much contamination, the preservatives won’t be able to handle it,” she warned. “You don’t want to play (about) with your eyes, right?”
The safety of other expired medicines “is also questionable”. She cited the commonly prescribed antibiotic, tetracycline. When it degrades, one by-product is anhydrotetracycline.
While this is unlikely to form before the expiry date under recommended storage conditions, “if you take expired tetracycline, the by-product … is toxic to the kidney”, she said. “It can cause kidney damage.”
When degraded, other drugs — not so much over-the-counter medicines as the high-level kinds — can also be dangerous for patients.
For example, insulin, used in the treatment of diabetes, breaks down quickly after the expiry date. If the insulin fails to treat or prevent blood sugar spikes effectively, complications could occur.
5. CAN YOU TELL IF A MEDICINE MUST BE DISCARDED?
There are ways, besides checking the expiry date, to determine whether a drug is no longer safe to consume.
“Smells do give us an indication,” said Chew, who cited aspirin as an example. “One of the by-products of aspirin degradation is acetic acid. Acetic acid is vinegar, so it’ll smell sour.”
Amoxicillin, an antibiotic used to treat bacterial infections, also has a smell — a “sulphur-like odour” — when degraded. A physical inspection can reveal another difference: The packaging would be bloated if the antibiotic is not good any more.

When a pill appears powdery, that is also an “indication that this drug isn’t safe”, Chew added.
6. SHOULD YOU TAKE DRUGS NOT PRESCRIBED TO YOU?
To clear out their supply of medications, some people have resorted to giving away or selling them at low prices in online marketplaces. A lot of the medicines are listed as new and within the expiry dates.
But it is illegal to distribute prescription medicine in this way, pointed out Ong, who cited the Medicines Act and the Health Products (Therapeutic Products) Regulations.
As for the online buyers, “it’s not advisable” to take those medicines, he said.
“What you’re doing is to skip the step whereby you see a healthcare professional, who’ll properly diagnose the problem and give you individualised advice on whether that medication is suitable for you (and) whether there are any side effects.”

While someone may share medication with a family member, “the same safety concern still applies”.
“For the pharmacy-only medications, we’ll ask you appropriate questions to assess (whether the health condition) is something that isn’t serious (and) you can treat on your own. Or is it something that may have an underlying issue?” Ong said.
If it is the latter, then a doctor’s diagnosis is needed, otherwise there is a risk of “masking” a bigger problem, he continued.
He cited the example of someone with gastric discomfort who buys off-the-shelf or pharmacy-only medication, which will treat the symptoms. “But maybe, underlying that, the problem that’s causing it is … stomach cancer or stomach ulcer,” he said.

With self-treatment, especially if it is someone else’s medicine, one must also be careful because pills may look the same, but the dosage could range, say, between 20 and 40 milligrammes.
For example, painkillers including paracetamol — which comes in many forms — may contain different amounts of the active ingredient inside.
“If you just remember the drug name, and you don’t check the actual dosage instructions, you may end up taking the correct number of pills, but the actual dose … is much higher than (what) it’s intended for,” Ong said.
Watch this episode of Talking Point here. The programme airs on Channel 5 every Thursday at 9.30pm.